Summit Exercises and Training LLC (SummitET®) experts will be presenting at the 34th annual National Radiological Emergency Preparedness Conference (NREP) in Dallas, Texas from April 29 to May 2, 2024.
The mission of NREP is “to provide a professional forum for individuals involved with the Offsite Radiological Emergency Preparedness programs to gather in the spirit of continuous self-improvement to share program experiences, develop solutions to common challenges, and create innovative planning, exercising, and training methodologies.”
SummitET offers multi-agency radiological preparedness exercises, trainings, and workshops for emergency planners and field personnel, led by our team of Strategic Communications experts, Certified Health Physicists, and Radiation Safety experts.
Join our expert sessions during the 2024 NREP Conference:
Keynote: “Using AI for Enhanced Radiological Emergency Preparedness Planning and Outreach: Emerging Threat or Emerging Opportunity?”
Session 8 | Tuesday, April 30, 8:30am

Holly Hardin
Director of Strategic Communications
Abstract
Artificial intelligence (AI) stands at the forefront of revolutionizing various aspects of our lives. AI’s ability to analyze vast amounts of data in real-time and its capacity for automation, predictive analytics, natural language processing, and image recognition are providing efficiencies and enhancements in all areas of preparedness. AI’s dynamic role in our lives is shaping how we plan for, respond to, and recover from evolving threats and complex challenges that demand a multifaceted approach to preparedness. However, these efficiencies and opportunities do not come without inherent risks and challenges. Ethical considerations and potential challenges associated with AI implementation to prepare for, respond to, and recover from a radiation emergency will also be addressed. At the end of this session, participants will gain an understanding of how AI is revolutionizing and shaping the future of radiological preparedness planning and outreach.
“Effectively Communicating With Patients and Healthcare Staff During a Radiological Event”
Steve Sugarman, SummitET
Ben Maltz, Washington Department of Health
Session 23 | Wednesday, May 1, 10:15am

Steve Sugarman, CHP
Vice President | Corporate Health Physicist
Abstract
Healthcare providers dealing with those involved in a nuclear power plant incident or other radiological emergency need to be able to understand the situation and make good decisions. Effective communication between health physicists and healthcare providers during a radiological emergency is critical to achieving positive treatment outcomes. Those tasked with medically managing victims of radiological incidents may be expected to have the same concerns as other members of the public when faced with a radiation event and may therefore have questions that could affect their willingness to respond or their ability to respond without the distraction of worrying about a misunderstood hazard.
Concerns that may need to be addressed include, but are not limited to: What are the risks associated with treatment of irradiated patients? Is it safe to admit a contaminated patient into the hospital? What are the priorities when treating a contaminated injured patient? How can I protect myself from radioactive materials?
Patient concerns are also an issue that needs to be addressed. Effective communication with patients and/or their families can have a significant impact on the healthcare organization. Examples of where effective radiological communications with patients/involved individuals play an important role for the healthcare institution: addressing an emergency room full of the worried-well, patient acceptance of prognoses or medical countermeasures, support at triage or population monitoring areas, and others.
While health physicists understand their roles include dose estimation, contamination control, etc., many do not understand their communication roles. Taking the time to develop good messages and effectively communicate with the involved individuals will ensure the healthcare provider understands the risks and priorities associated with a radiological response and the patient understands the implications of the radiation dose they may – or equally as important – may not have received.
“Readability and Accuracy of DRDs at Low Doses of Radiation”
Angela Leek, SummiET
Scott Wendt, Iowa State University
Session 28 | Wednesday, May 1, 1:55pm
“Decoding the Response: Leveraging Mental Models in Radiological Emergencies”
Session 40 | Thursday, May 2, 2:15pm

Angela Leek, PhD, CHP
Director of Radiological Solutions and Regulatory Affairs
Abstracts
Readability and Accuracy of DRDs at Low Doses of Radiation
The 2019 REP program manual suggests that offsite response organizations provide emergency workers (EWs) with two direct reading dosimeters (DRDs): a low range and a high range. This recommendation is based on the observation that higher-range dosimeters, like those reading 0-SR or 0-20R, might not show changes at the 500mR dose level. There’s concern that such dosimeters might lead a responder to receive their maximum allowed dose of 5 rem before noticing any accumulated dose. This risk arises from applying correction factors, often around 5 times, to account for internal doses. In contrast, lower-range DRDs, which are believed to reflect lower doses more accurately, might max out before reaching the dose limit. Thus, the two-dosimeter approach is suggested.
However, there are limited scientific data about high-range DRDs’ capability to detect and display doses at the lower end of their scales. Furthermore, few studies gauge how well emergency workers can spot minute changes below the 1 R level on high-range DRDs.
Our study assesses the response of high-range pencil dosimeters and their readability, especially for responders unfamiliar with radiation environments. Issuing two DRDs might be challenging operationally; emergency workers could face confusion about which to read or report, potentially adding to the stress of their tasks.
In this follow-up presentation from one made at NREP in 2023, we’ll present data gathered from the general public, representing emergency workers at a NPP incident. These participants were tasked with reading high-range DRDs exposed to low radiation doses to assess their ability to accurately read each dosimeter at low exposures (below 1 R).
Decoding the Response: Leveraging Mental Models in Radiological Emergencies
Imagine standing at the precipice of a radiological emergency—where the knowledge you hold and the myths you believe could spell the difference between control and catastrophe. This is where our recent research kicks in, revealing a reality that isn’t surprising to most who have been in the field for a while: the mental model of emergency responders, their grasp on radiation and risk, can have a significant impact on how they respond. Those who have confidence in their training and in the leaders directing them more effectively executed expected response procedures. But there’s a catch: if they have the wrong idea about the risks of radiation—for example, thinking that a 25-rem dose is more dangerous than it actually is—their performance takes a hit.
It’s time to take a close look at what misconceptions our current approach to training may be subtly reinforcing. Ask yourself: Are the myths of radiation fully dispelled in your training? Is your own knowledge influenced by ingrained fallacies? Using insights from this recent study and a tool called
the EMMS Diagnostic Matrix, we’re set to reshape our understanding of emergency response behavior. But knowing is only half the battle; the real challenge lies in applying this knowledge to develop more effective training methods, perhaps through virtual reality experiences, and then evaluating their effectiveness. This session is more than a presentation—it’s an invitation to learn how we can use innovative approaches to improve our understanding of responders’ training needs and our collective approach to radiological risk perception.
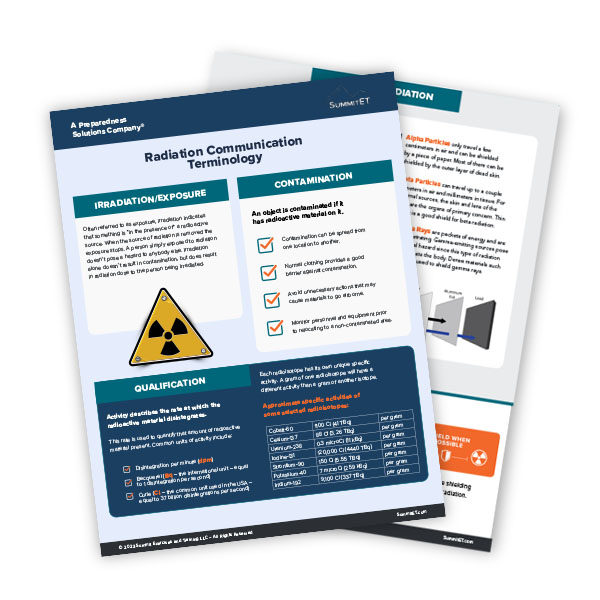
Radiation Industry Tools
Request a Meeting With Our Experts
Or Pick a Meeting Time
See Upcoming Events
Our experts are consistently in the field at conferences and trade shows to stay on top of industry trends and innovative preparedness solutions. Find out where our team will be next and schedule a meeting.
Radiation Communications Resources
SummitET News
SummitET to Offer Free Strategic Communications Webinar to Empower Institutions of Higher Education to Navigate Sensitive and Controversial Issues
Summit Exercises and Training LLC (SummitET®) is pleased to announce a free upcoming virtual workshop titled "Strategic Communications for Institutions of Higher Education: Navigating Sensitive and Controversial Issues." This webinar is specifically designed for...
SummitET Celebrates 10 Years of Success and Innovation
St. Petersburg, FL – Summit Exercises and Training LLC (SummitET®), a Preparedness Solutions Company®, is proud to announce the celebration of its 10th anniversary this month. Since 2013, SummitET has been a driving force in the preparedness services industry,...
SummitET Graduates from MissionLink’s 2023 Cohort; Joins Esteemed ‘Trusted Innovation Ecosystem’ in NatSec Tech
November 16, 2023 | St. Petersburg, FL – Summit Exercises and Training LLC (SummitET®) a Preparedness Solutions Company®, is proud to announce that John Duda, CEO, has graduated from MissionLink, an exclusive nationwide network that serves as a force-multiplier and...